[CANCER] Where has the last week+ gone?

So, I last blogged 30th Jan, saying that breathlessness was becoming a big problem, but I was waiting for CT scan at the Christie (where they can use my portacath), and a biopsy for chest rash with surgeon at Wythenshawe. My head is spinning somewhat - but I find blogging about stuff a helpful […]
[CANCER] Participation in Trials

Within the last 3.5 years, I have been involved in a a number of cancer-related trials (clinical trials and quality of life trails are both important): Optima This trial is looking at testing tissue samples to try and find if you might benefit from having chemotherapy to treat your breast cancer: there is a sense […]
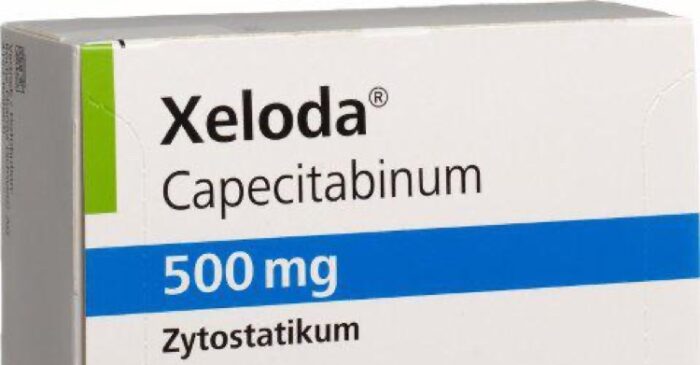
[CANCER] Time to Start Capecitabine

It’s not even a week since I updated about my cancer situation, but here’s a little more information. Capecitabine is a type of chemotherapy called an anti metabolite. The body changes capecitabine into a common chemotherapy drug called fluorouracil. It stops cells making and repairing DNA. Cancer cells need to make and repair DNA so […]
[CANCER] A rather exhausted update
It was only a couple of weeks ago that I updated everyone as to where we were at on treatment, that I’d had a pleural effusion (fluid on the lungs) identified, though oncologist thinks that it’s the toxicity of the treatment causing breathing issues, rather than the effusion itself .. Still very tired, planned to […]
[CANCER] New Treatment?, Treatment Break and Pleural Effusion #BusyLivingWithMets
I last blogged a couple of weeks ago, when I’d been sent home, breathless, without treatment. I had hoped that a treatment break would mean that I felt amazing, but, although my skin has cleared up a lot, and a lot of sensation has returned to my hands/fingers (not all!), mostly I still feel super […]
